
UTSW
By Yair Lotan, M.D. Urology
We’ve all seen the sitcoms where the male lead is given an ultimatum: Get a vasectomy or say goodbye to sex. He freaks out, digs in, hilarity ensues, and eventually he decides to get the procedure – only to discover it was quick, easy, and much less scary than he thought.
In real life, most patients are far less dramatic. But that last part is true. Vasectomy is a safe, relatively simple procedure that is more than 99% effective at preventing pregnancy.
In fact, vasectomy, which blocks the release of sperm during ejaculation, is one of the most cost-effective ways to prevent pregnancy – it’s a one-time, outpatient procedure that most insurance companies cover. Vasectomy does not interfere with testosterone production, sexual function, or ability to urinate. The surgery can even be reversed in some cases, though it is intended to be permanent.
More than 500,000 vasectomies are performed each year in the U.S.
Men considering vasectomy, or even those just curious about it, should talk with a urologist, a doctor who specializes in the male urinary system. We’ll explain the procedure and answer your questions. If you choose to move forward with a vasectomy, we want you to feel confident and committed to the decision.
How vasectomy works
Vasectomies are usually performed in the doctor’s office or clinic.
During initial conversations with your urologist, you’ll decide whether you will need to be fully sedated for the procedure. Many vasectomies are completed using only local anesthetic that numbs the surgical area, but in complex cases general anesthetic can be used. You should arrange for someone to drive you home following the procedure if you get anesthesia, but most men can drive themselves home if they just get a local anesthetic.
Your doctor will advise you to avoid aspirin, blood thinners, and nonsteroidal anti-inflammatory drugs such as ibuprofen for at least 48 hours prior to the procedure to reduce your risk of bleeding. Be sure to discuss any medications you are taking with your doctor.
Just prior to the procedure, your scrotum will be shaved and washed with an antiseptic solution. If you’re receiving local anesthetic, this will be injected to numb the area, blocking any sharp pain.
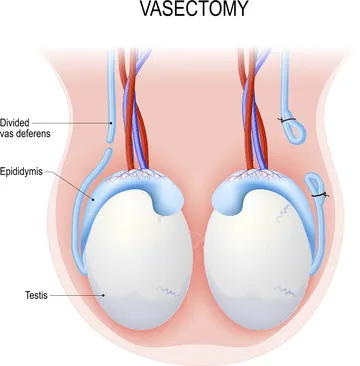
The doctor will make a small incision in your scrotum on each side and retrieve the vas deferens – the tube through which sperm travels from the testicles to the urethra. The doctor then cuts the vas in two, and both ends of each tube are surgically sealed before being placed back inside the scrotum. The incisions in the scrotum are sealed with stitches or allowed to heal on their own.
Most patients return home immediately after the procedure. It is common to feel some discomfort for a few days. You may take over-the-counter medication such as Tylenol, Aleve, or Motrin to help. Swelling and pain can be reduced with an ice pack applied 20 minutes at a time – harkening back to our sitcom scenario, a bag of frozen vegetables can be an effective ice pack substitute. A scrotal support or jock strap to elevate the scrotum is recommended for one to two weeks.
Avoid sex and ejaculation for a week after the procedure. When you resume sex, use backup birth control for at least 12 weeks or longer, depending on your doctor’s recommendations. Most men can return to work the next day, though you’ll want to avoid strenuous activities such as jogging and strength training for approximately a week.
Complications from vasectomy are rare. There is a slight risk of post-vasectomy pain syndrome, which occurs in fewer than 2% of men. It is usually treatable with medication.









